Course of LABORATORY MEDICINE
The Catabolism of the Heme
Some 400 mg of heme are degraded and excreted daily by healthy adults as bilirubin derivatives. Over 70% of the heme derives from the turnover of hemoglobin (i.e. from aged erythrocytes or erythrocyte precursors), the rest from other hemoproteins present in all the body cells.
Free heme is toxic because of its ability to activate O2 to superoxide and peroxide anions. It is transported in the blood plasma bound to hemopexin or albumin and removed by the cells of the reticuloendothelial system, in the liver or elsewhere. The same cells are able to endocytose and degrade aging red cells. Reticuloendothelial cells degrade the heme with the enzyme heme oxygenase, that opens the tetrapirrole ring and releases iron (which is recycled). A product of this reaction is the toxic gas CO; this is the only reaction known to produce CO in our body. The heme derivative thus obtained is called biliverdin and is further processed to bilirubin by the enzyme biliverdin reductase.
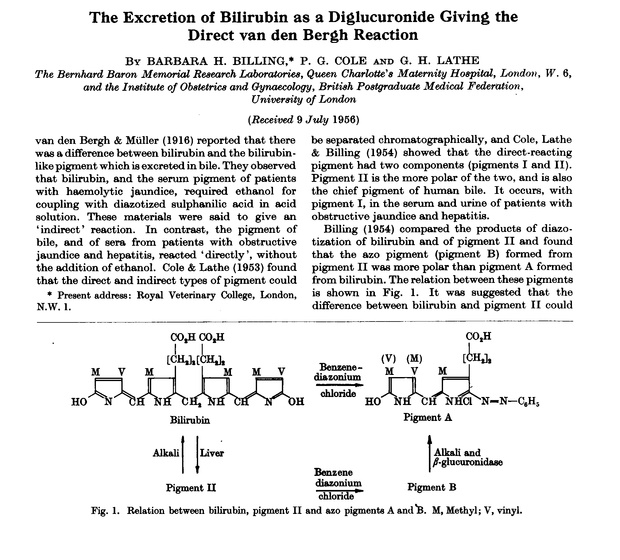
Bilirubin is water insoluble and when it is released by the reticoloendothelial cells, is taken up by albumin and carried to the liver (many reticuloendothelial cells do actually reside in the liver). Glucuronyl transferase, an enzyme of the hepatocyte, conjugates one or two molecules of glucuronic acid to bilirubin. The reaction products, bilirubin-glucuronide or bilirubin-diglucuronide, are soluble in water and are excreted via the bile in the faeces.

During the intestinal transit, bilirubin is partially metabolyzed by the bacterial flora and converted to other pigments called stercobilinogens and urobilinogens, thay may be partly readsorbed by the gut and excreted in the urine. Bilirubin and the bilinogens are of a brownish colour, and are responsible for the colour of the faeces. If readsorbed and excreted in the urine, they cause the urine to become dark brown.
Bilirubin is normally present in the human blood, in two forms: (i) unconjugated bilirubin is bound to albumin and is present during its transfer from reticuloendothelial cells to the liver. This form of bilirubin is also called indirect (because it requires ti be activated in order to react with the standard diazo reagents) or pre-hepatic. (ii) Conjugated bilirubin is present in the blood because of reabsorption from the smallest biliary vessels. This form is also called direct or post-hepatic.
JAUNDICE (or ICTERUS)
In the healthy adul the total serum concentration of bilirubin is <1 mg/dL, mostly due to unconjugated bilirubin in transit from the spleen or other reticuloendothelial system sites to the liver. Conjugated bilirubin is <0.3 mg/dL. In the newborn, especially the premature newborn, the serum bilirubin may be significantly higher, up to 5-7 mg/dL.
Bilirubin concentration may be increased because of several reasons; above 2 mg/dL it causes a yellow staining of the eye sclera, the skin and all visible tissues rich in elastin, to which it binds (e.g. the frenulus of the tongue). Ths condition is called jaundice.
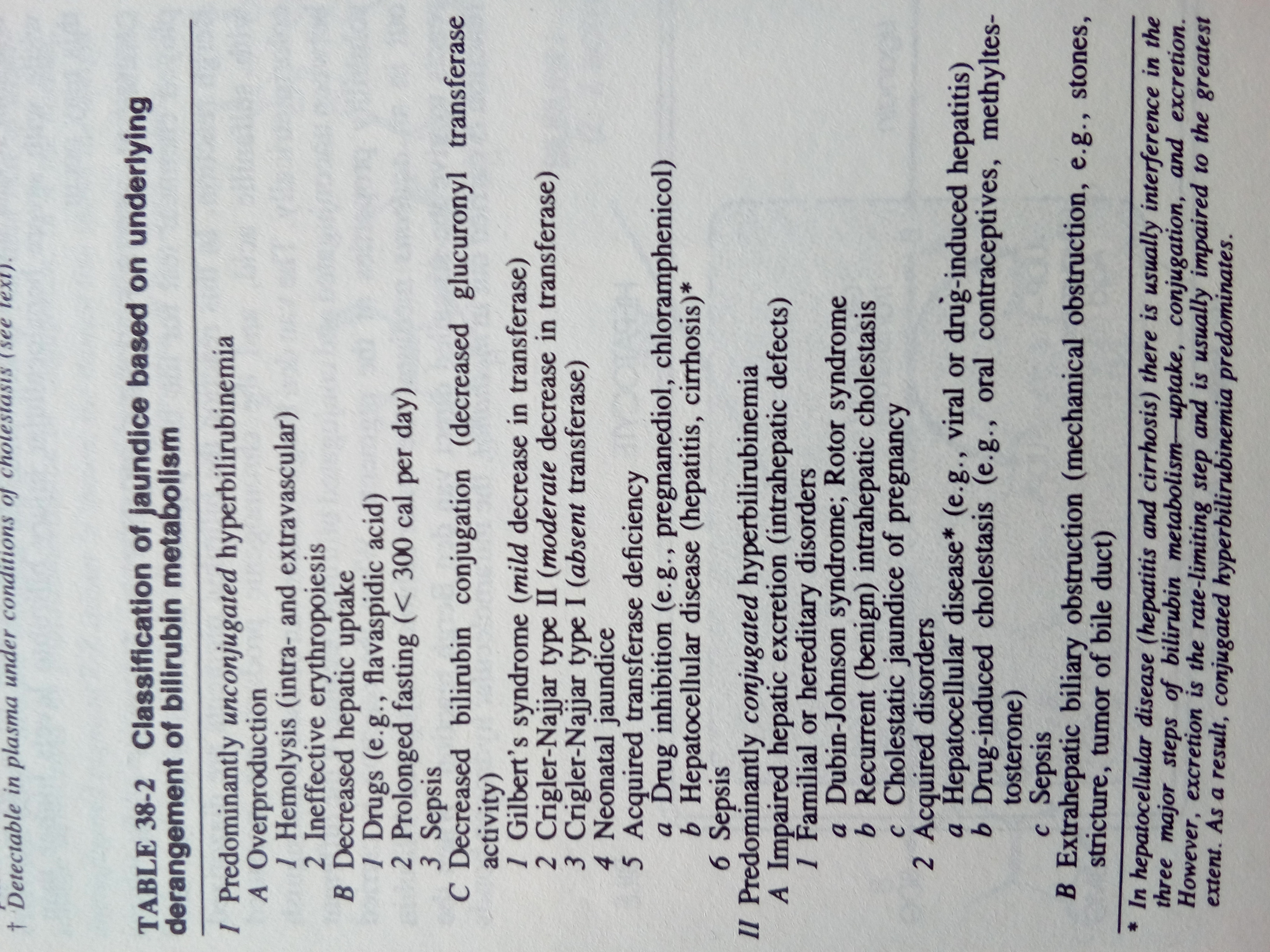
| Bilirubin type | Possible causes |
| unconjugated | hemolysis Gilbert's syndrome (congenital, benign) Crigler-Najjar syndrome type I (hereditary, autosomal recessive, lethal) Crigler-Najjar syndrome type II (hereditary, autosomal dominant, severe) Primary shunt hyperbilirubinemia (familial, benign) |
| conjugated | Dubin-Johnson syndrome (hereditary, autosomal recessive, benign) Rotor syndrome (hereditary, benign) |
| both | intrahepatic cholestasis, causing bile reabsorption in the blood. May occur because of cholelithiasis, hepatitis, cirrosis, biliary cancer, etc. |
LABORATORY EVALUATION OF LIVER FUNCTION
Jaundice is a common sign that may be caused by a host of diseases (see Table). It is a generic clinical sign, that may accompany a host of hepatic conditions (and some non-hepatic ones); the diagnosing the underlying disease is usually based on a series of clinical tests ordered sequentially to exclude or ascertain the different possibilities. Jaundice occurring in an adult patient is first evaluated by ascertaining two points: which type of bilirubin is increased, and whether the condition is acute or chronic. In the presence of jaundice (even mild jaundice), laboratory signs of liver damage should be systematically looked for.
Serum bilirubin concentration: in the healthy adult does not usually exceed 1 mg/dL, of which one third is due to conjugated bilirubin and the remaining two thirds to unconjugated bilirubin. Jaundice becomes visible (initially in the sclerae) when bilirubin concentration in the serum exceeds 2 mg/dL. Unconjugated bilirubin is mostly bound to albumin and must be solubilized with organic solvents for the test. The standard test for bilirubin is based upon the reaction of this compound with p-diazobenzenesulfonic acid (van den Bergh reaction); the reaction product is red-colored and can be measured by absorption spectrophotometry. This reaction transfers the diazo-dye to bilirubin:
Bilirubin conjugated with glicuronid acid reacts with diazo-compounds in water and is thus called "direct" bilirubin; the reaction of unconjugated bilirubin requires that ethanol is added as a co-solvent, thus unconjugated bilirubin is also called "indirect" bilirubin.
Conjugated bilirubin is water-soluble and is filtered by the kidney; it causes the urine to be yellowish. In case of obstructive jaundice and cholestasis, conjugated bilirubin is reabsorbed in the serum and causes the urine to become dark, whereas the faeces become paler.
Aminotransferases: aspartate aminotransferase (AST, GOT) and alanine aminotransferase (ALT, GPT) are intracellular enzymes present in several tissues, but most notably in the hepatocytes. Diseases that cause necrosis of hepatocytes (e.g. viral hepatitis, cirrosis, liver cancer) they are released in the serum. Their serum concentration in the healthy adult is non-zero may because of the physiological turnover of liver cells but should not exceed 40 u/mL; in viral hepatitis may exceed 400 u/mL. Jaundice is often associated to increase of aminotransferases, but the reverse is not true, because of two reasons: (i) liver damage may be sufficient to yield a significant increase in the enzymes, but insufficient to cause a significant increase of bilirubin concentration; and (ii) damage of tissues other than the liver may cause increase of the aminotransferases (e.g. the heart and the central nervous system).
If viral hepatitis is suspected, the viral antigen, antiviral antibodies and viral DNA may be looked for. Viral hepatitis A is transmitted by contaminated food and water, has short incubation time and is relatively benign; the characteristic viral antigen HAAg is found in the serum, stool and liver tissue. The disease runs an acute course and there is non chronic carrier state; occasionally it may cause epidemic outbreaks in regions with poor sanitation.
Viral hepatitis B is transmitted by blood transfusions and contact with infected blood, runs an acute course but may chronicize and is associated to chronic hepatitis and liver cancer. Diagnosis is established by the finding of the specific viral antigens HBsAg (Australia antigen), HBcAg, HBeAg and the delta antigen.
Viral hepatitis C resembles B under many aspects but is due to a different virus. Diagnosis relies on the demonstration of specific antibodies by immunassay, or on the sequencing of viral RNA from the serum samples.
Alkaline phosphatase is characteristic of the biliary duct cells and is increased in many cases of obstructive jaundice and liver cancer. Other organs that may release this enzyme in the serum are pancreas, lung and bone.
gamma-Glutamyl transpeptidase is increased in many cases of liver disease (e.g. ethilism, drug toxicity, etc.).
Other tests: if an obvious anatomic lesion is suspected (e.g. biliary cancer, cirrosis) imaging methods (MRI, echography) and liver biopsy should be considered.
Slides of this lecture:
 |  |
 |  |
 |  |
 |  |
Home of this course